This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
THORACIC OUTLET SYNDROME
Thoracic Outlet Syndrome
Thoracic Outlet Syndrome early treated
Thoracic outlet dynamic phlebography
DESCRIPTION
What is Thoracic Outlet Syndrome?
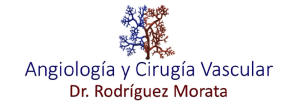
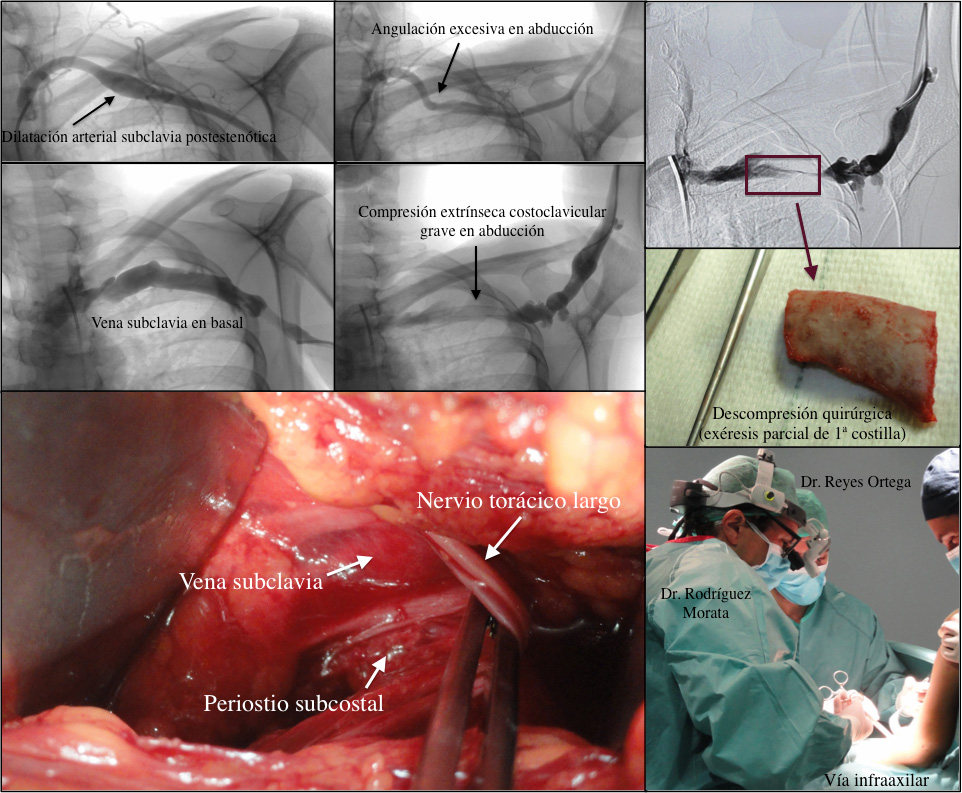
The manifestations produced by chronic compression that take place in blood vessels and/or nerve stems which cross from the arm to the thorax towards one or other direction. These compressions may arise between the clavicle and 1st. rib, or either under the pectoralis minor muscle. The pathology caused by all of this is generically called “Thoracic Outlet Syndrome” (also known as Thoracic Operculum Syndrome).
The alterations may be produced at the level of the subclavian artery (aneurysms, embolisation, hand ischemia) of the subclavian vein (deep vein thrombosis) or of the brachial plexus (chronic pain and numbness of the internal side of the hand, forearm and changes with different postures).
What is Paget-Schroetter syndrome?
This syndrome, also known as Effort Vein Thrombosis, is caused by thrombus acute occlusion at subclavian vein level, between the clavicle and the 1st. rib exactly. That thrombosis is originated because the subclavian vein suffers chronic trauma at that level and if the anatomical space is slightly more reduced than what it commonly is and there is an individual predisposition, that continuous trauma makes the vein, chronically damaged, become finally thrombosed.
However, that subclavian vein thrombosis may also be due to large calibre catheters placement in its inside, for haemodialysis, chemotherapy treatments or prolonged parenteral nutrition. In these cases, costoclavicular pinch-off has nothing to do nor repeated compression and therefore this is not part of Paget-Schroetter syndrome, rather it is simply called secondary Subclavian Vein Thrombosis.
What symptoms does it cause?
The usual manifestations of this subclavian vein thrombosis are abrupt elastic limb edema occurrence, with musculature compaction, moderate pain and arm and forearm slightly warmer and subcyanotic. Moreover, a typical history of continuous effort in sporting or working settings use to match in 80 % of the cases and therefore are more common in dominant upper extremities, usually in young patients. As in any vein thrombosis, this one may be continued with pulmonary thromboembolism (pulmonary embolism) although less frequently than in lower extremities vein thrombosis.
How is Thoracic Outlet Syndrome treated?
In the acute moment of vein thrombosis, the response to fibrinolysis with catheter is often highly favorable in the first two weeks (mostly in the first 8 days), with a success rate of 80% in thrombus total lysis and currently is the first choice treatment, above conservative treatment. Already with vein patency, we can subsequently perform angioplasty of the chronically injured area, even sometimes, placing a stent (only in absolutely necessary cases), and thoracic outlet decompression after it: to increase the space so that the vein does not narrow again due to compression between the rib and the clavicle. We usually perform first rib resection to this effect in its most anterior and medial area transaxillary in order to widen costoclavicular space.