This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
COMPRESSIVE VASCULAR SYNDROMES
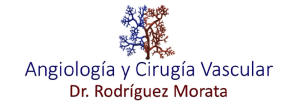
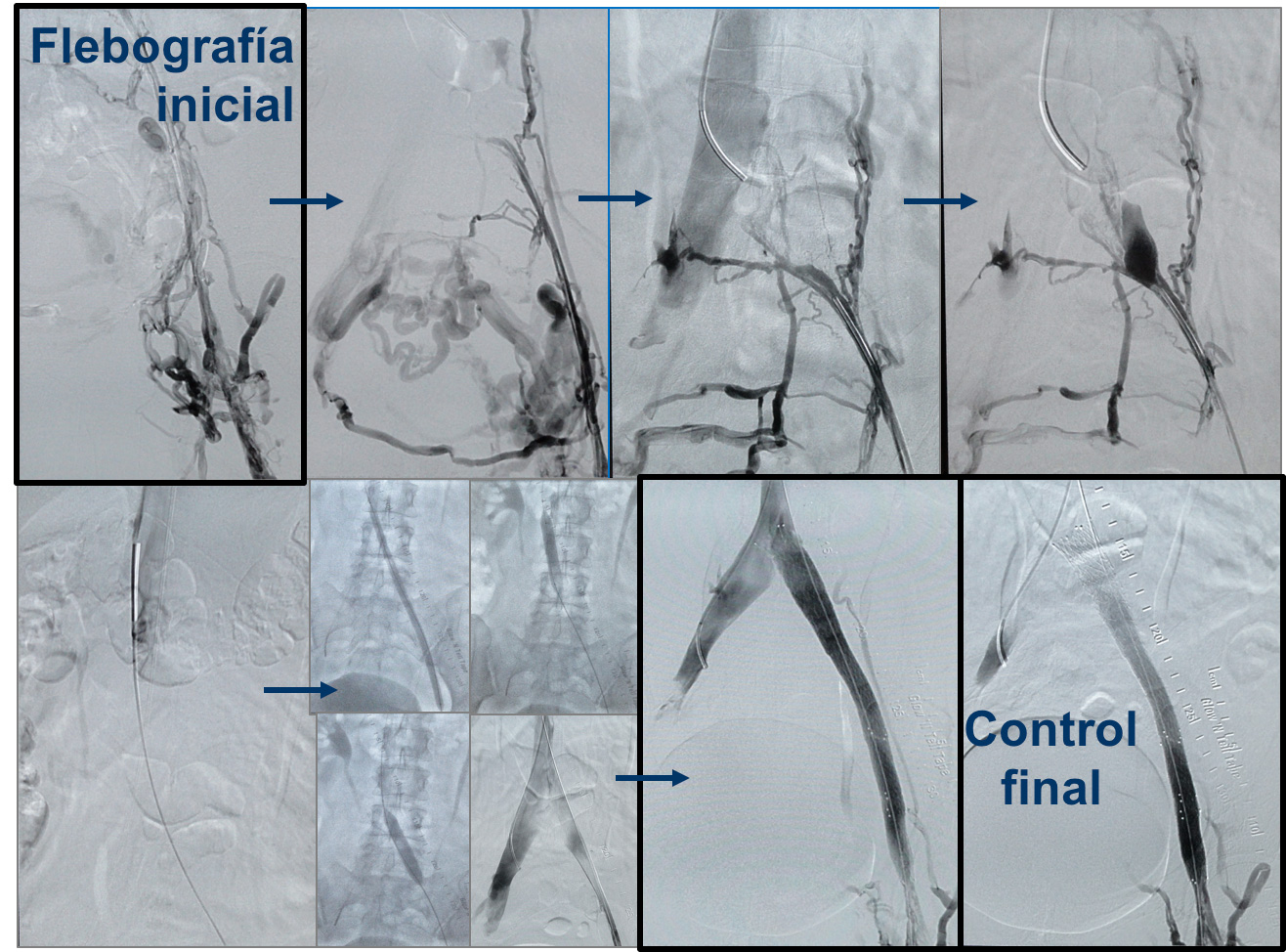
Implante de Stent en Sd de MAY-THURNER
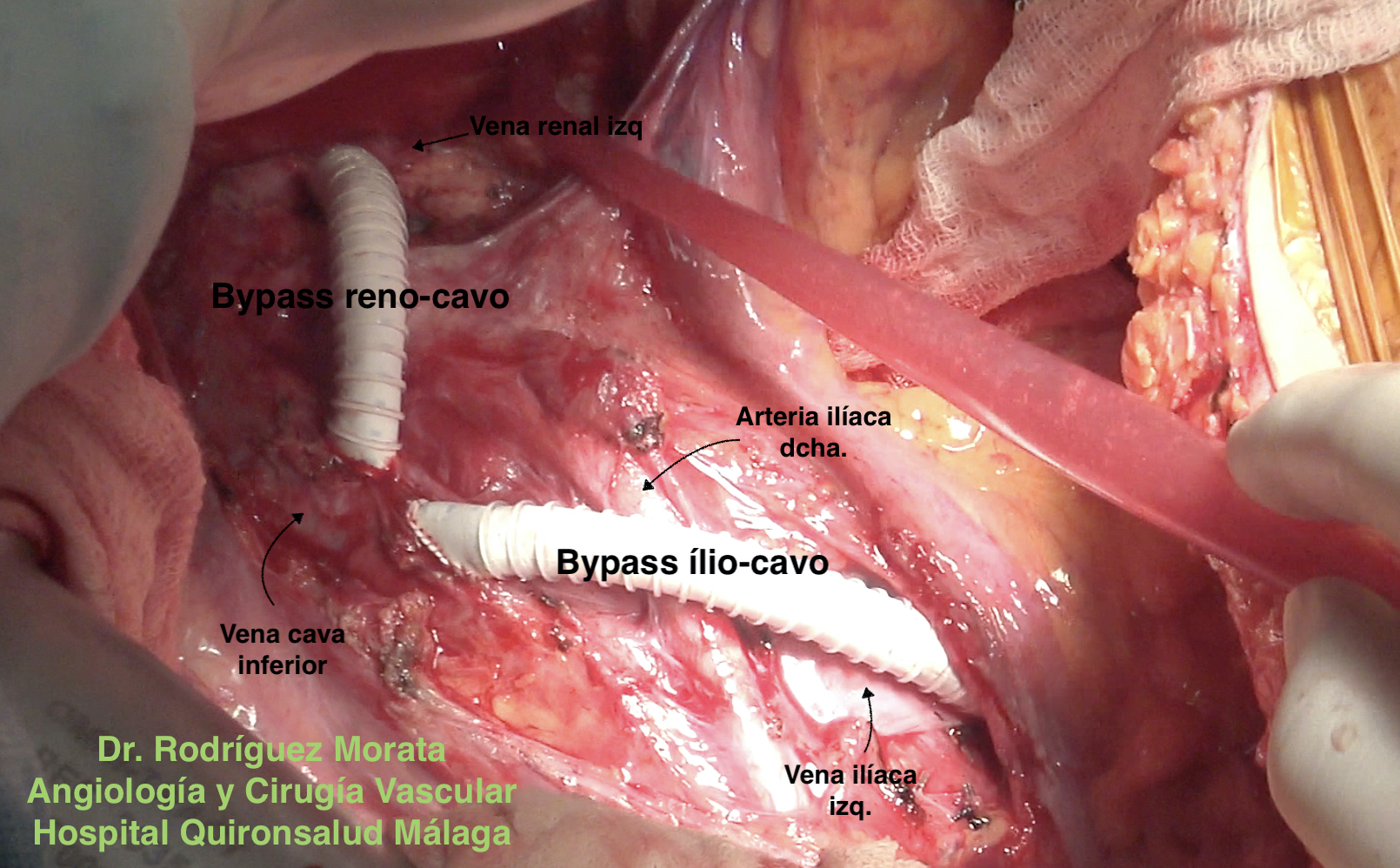
Trasposición de vena renal izquierda
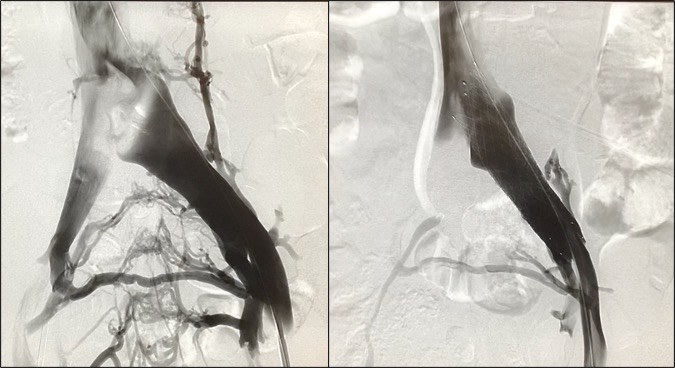
Cirugía abierta síndromes compresivos
Bypass en síndrome de May-Thurner
Bypass en síndrome de Nutcracker (Cascanueces)
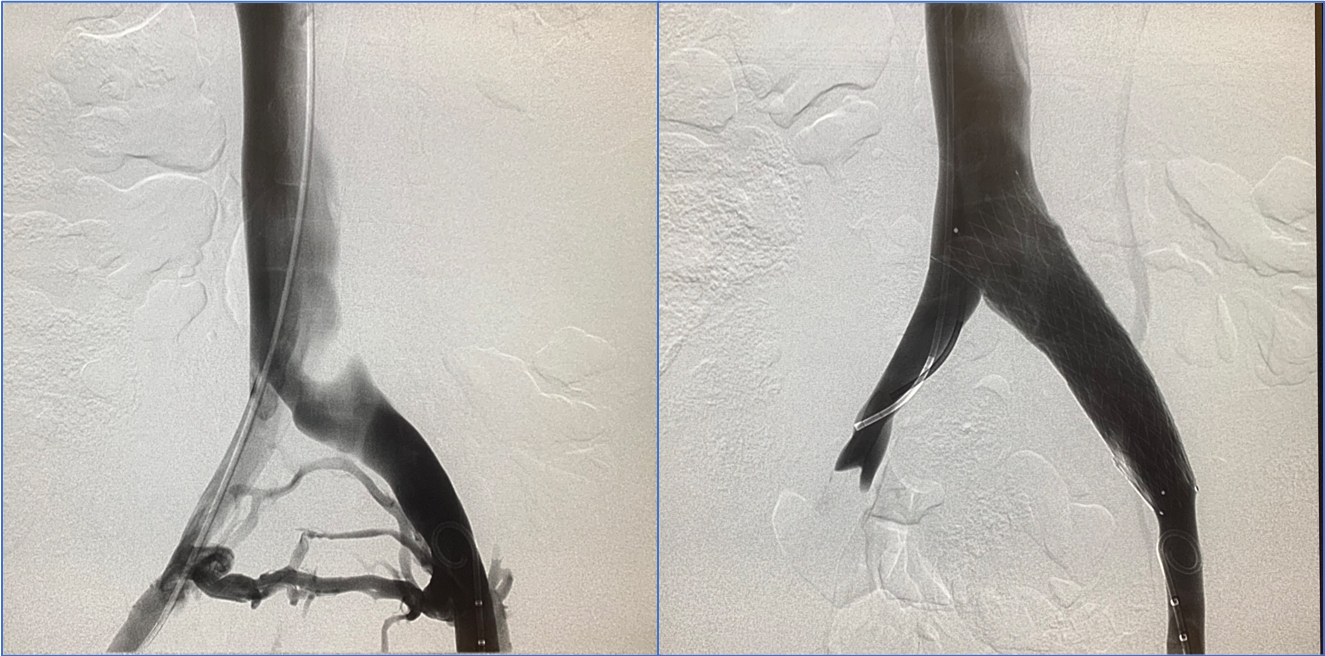
Trombosis venosa profunda iliofemoral. Síndrome de May-Thurner
Phlebography versus Vascular Ultrasound
Stent vena ilíaca en Sd May Thurner
Left Eagle Syndrome
Kidney autotransplant in Nutcracker Sd.
DESCRIPTION
What is a compressive syndrome?
The constellation of symptoms and signs that have as their origin the extrinsic compression of a vascular structure. Under this denomination we can refer to the compression of an artery such as the celiac trunk (Middle Arcuate Ligament Syndrome) or of major venous compressions, typically Nutcracker or Nutcracker Syndrome and May-Thurner Syndrome. When we talk about compression syndromes, we don’t mean compression caused by tumors.
Why do we talk more and more about compressive venous syndromes?
Because they are frequent, more and more of them are known and each time we have better diagnostic methods. However, many times it can fall into an excess of diagnosis based on inaccurate imaging tests and an excess of treatments can occur without a clear indication. These pathologies require a high level of specialization to achieve a good result with their treatment.
Are compressive syndromes usually associated?
Yes and in fact it is highly frequent. It is common to observe a venous compression at the level of the left renal vein and the left iliac vein, since these structures must cross from the left to the right side and pass over the spine or aorta to reach its drainage in the inferior vena cava. And that is the weak point of these great veins. In fact, practically all people have some degree of compression, but something physiological, not a compression syndrome. This is one of the great challenges of diagnosis: distinguishing the merely physiological or a simple finding in an imaging test, from the truly pathological.
However, the fact of associating does not mean that both syndromes have to be treated or done together at the same time. Each case must be individualized.
What is Nutcracker or Nutcracker Syndrome?
When an image test shows a marked compression of the left renal vein between the aorta and the superior mesenteric artery, the patient is often referred to us for a possible Nutcracker Syndrome. But this is nothing more than a find. To this, the specialists in Angiology and Vascular Surgery usually call it a pseudo-Nutcracker or false Nutcracker at first until we show that there really is real compression and that it generates hemodynamic changes. It is absolutely essential to differentiate these findings from what a true Nutcracker Syndrome represents, which generates a whole constellation of symptoms and signs easily recognized by a specialist in Angiology and Vascular Surgery.
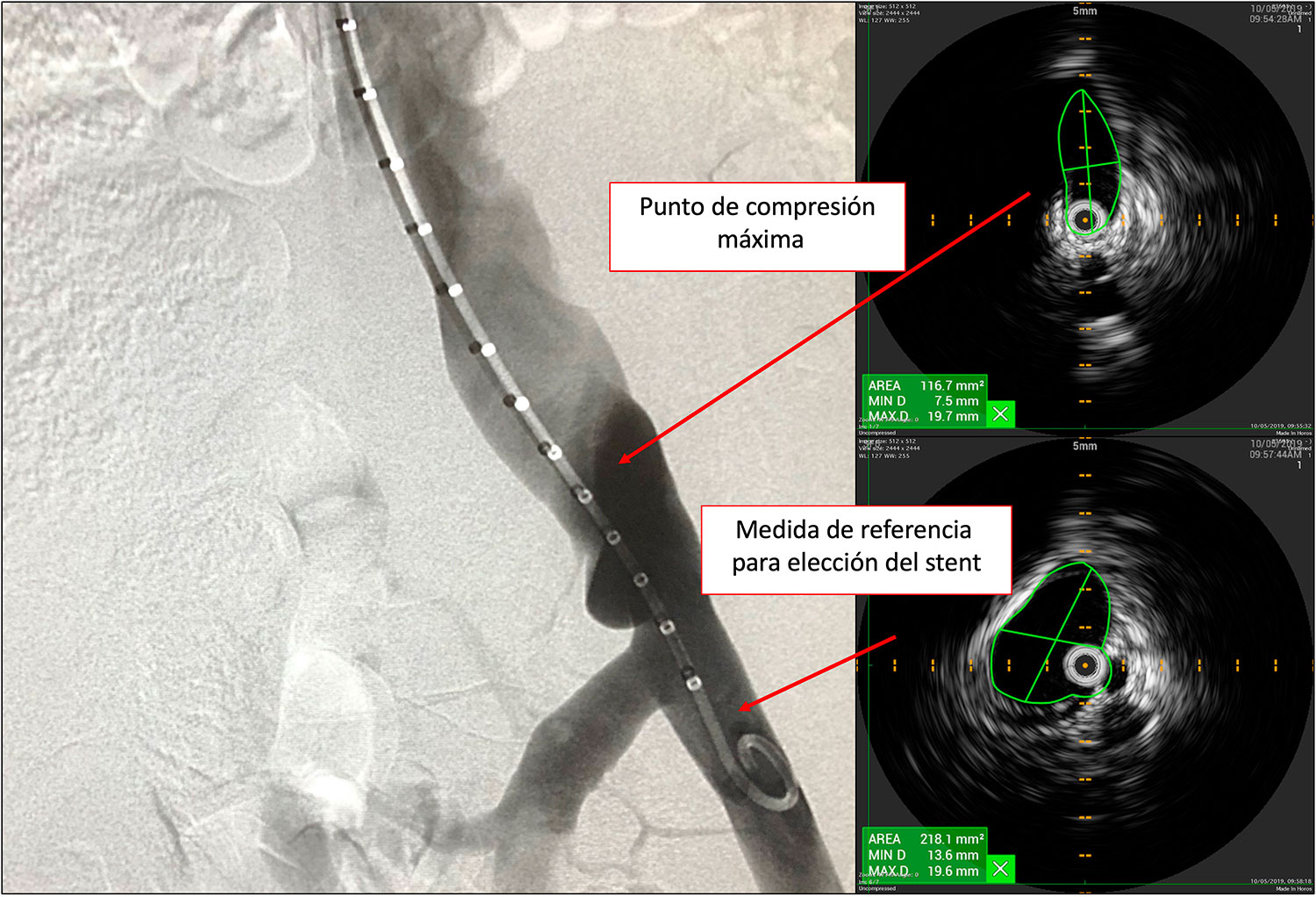
In addition to the clinical aspect there are a series of tests that can be requested, but that can never diagnose this pathology with certainty, and are Doppler ultrasound, resonance and CT. They can make us advance a lot in the diagnosis or discard of this pathology, but the only thing universally accepted today as a true diagnosis of Nutcracker with real compression is intravascular ultrasound (IVUS). In case of not having this technology, in many cases it can be diagnosed with pressure taking during phlebography within the renal vein and vena cava, but the standard gold method is IVUS.
How is Nutcracker Syndrome treated?
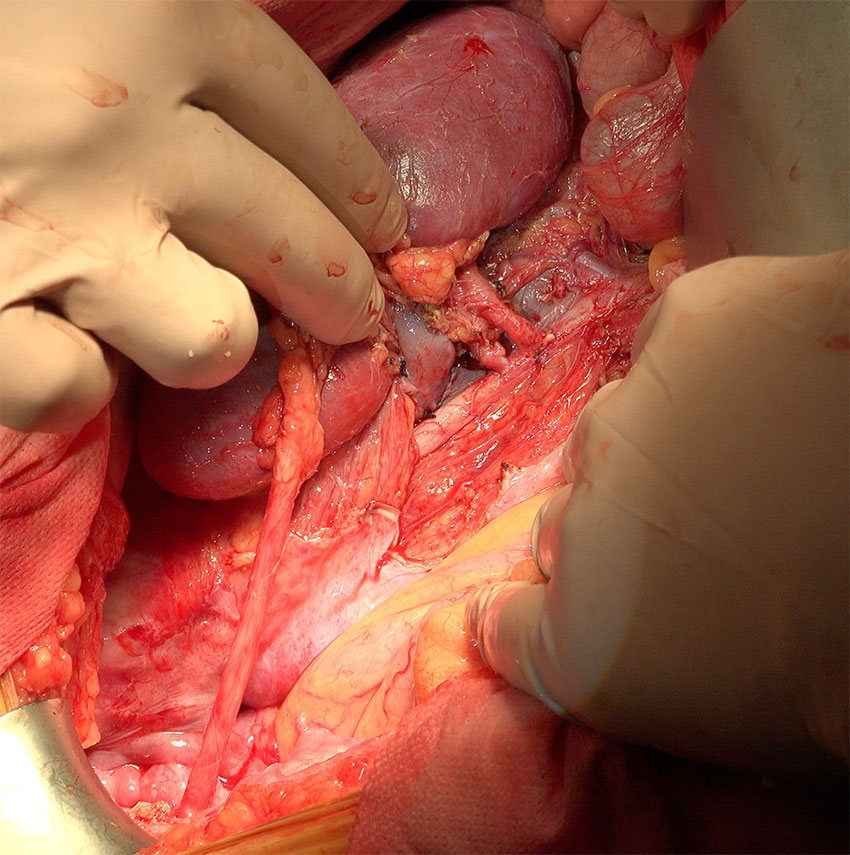
If it does not improve from a conservative point of view, which sometimes does, you have to think about a derivation of blood from the renal vein into the vena cava. Until a few years ago we considered that the first indication was the implantation of a stent inside the renal vein, but in view of the results and potential complications, currently the most accepted among the specialists who treat this pathology (Angiology and Vascular Surgery) is to perform an open bypass surgery (transposition, bypass, etc). There are other techniques such as the external stent but they are completely experimental.
What is a May-Thurner syndrome?
It is the pathological compression of the iliac vein, usually on the left side, between the spine and the right iliac artery. This May-Thurner syndrome is the cause of the vast majority of proximal deep venous thrombosis of the left lower limb. In these cases, when thrombosis has already occurred, the sequelae and treatment are more complex than if this syndrome can be diagnosed before a venous thrombosis occurs. The symptoms that give a pathological compression of the left iliac vein (before thrombosis) are usually a tension or congestive sensation of the limb that increases with exercise and even forces the patient to stop, and can cause secondary pelvic venous disorders with the usual known symptoms (pelvic congestion, chronic pain, etc.). Secondary varicose veins may also appear in the groin, genital or pelvic area.
The treatment of May-Thurner syndrome before it can be complicated is the implantation of a stent inside the diseased vein, to dilate the narrow area. Classic surgery is not chosen at the outset because it is too aggressive in relation to endovascular treatment, although it is also an option that we can consider in some cases (ilio-cavo bypass).
Who should treat these pathologies when it is necessary to intervene?
Keep in mind that when treating a disease, the best specialist is one who can handle all options: open or endovascular. If a specialist only handles one of the two options, he will not be able to offer different alternatives to a patient, unless he is referred to a different specialist, and therefore it is possible that he always tends to opt for only the option he manages and not everything is worth for all cases.
Without a doubt, the best option for any vascular pathology is to have a specialist who treats these pathologies with all possible options: the Angiologist and Vascular Surgeon.
What is Wilkie Syndrome?
In all patients with an aorto-mesenteric clamp, there is compression to a greater or lesser extent of the duodenum in its third portion as well as of the left renal vein, but both compressions are not usually equally severe. When the predominant symptoms are due to compression of the left renal vein, we have Nutcracker Syndrome (Nutcracker). These types of patients usually always notice gastric filling (they feel very bloated when they eat even a little), but it is not for this reason to assume that the duodenum is semi-obstructed, far from it. And vice versa, patients with severe stenosis of the duodenum (due to the aorto-mesenteric clamp) usually present many digestive symptoms, but not of the left renal vein. Let’s not forget that each patient is different even with similar pathologies.
Usually in cases of severe stenosis of the duodenum due to compression of the superior mesenteric artery in the aorto-mesenteric clamp (Wilkie syndrome), the surgical treatment that can be performed is a duodenojejunostomy, done by specialists in Digestive System Surgery. If the patient also has compressive vascular syndromes, in some circumstances, we could consider joint surgery, although the strategy of two different times is the usual one. Each case requires a detailed study.
What is the Arcuate Ligament Syndrome?
It is a very particular cause of chronic intestinal ischemia and is not due to arteriosclerosis or the previously mentioned pathologies. It is due to chronic compression of the median arcuate ligament on the celiac trunk. This ligament is a thickening in the form of a true tendon in some muscle fibers of the insertions of the diaphragm muscle, on either side of the abdominal aorta, just at the level of where the celiac trunk originates. This ligament is located exactly above this artery and slowly compresses it, producing a chronic injury whose end is usually the obstruction. This compression syndrome is very rare, but it must be considered among the causes of chronic abdominal pain in young people.
The treatment of this syndrome has two objectives: to surgically decompress this artery, releasing the ligament and the adjacent diaphragm pillars, and to revascularize the diseased artery, to avoid its obstruction (aorto-celiac bypass or stent in the celiac trunk, depending on the case). Treating this syndrome by implanting a stent, without prior surgical release, is usually not effective, since compression on the stent usually ends up breaking it and thrombosing the artery.
Other rare but disabling causes of chronic pelvic pain
Many patients with chronic neuropathic pelvic pain consult in Angiology and Vascular Surgery. They usually have intense, disproportionate pain, of an electrical nature, in the form of cramps and without a defined rhythm. They usually have multiple imaging tests (resonances, CT, etc.) where nothing is usually found. The tests that can contribute something are the magnetic resonance with neurographic sequence, the transvaginal or transrectal ultrasound, and sometimes a laparoscopy itself with therapeutic intent.
These patients may well report symptoms of refractory pelvic and perineal pain, constant vulvodynia, constant anal sphincter pain with no fissures present, and the underlying cause usually responds to nerve entrapments of the intrapelvic portions of the somatic or autonomic nerves.
This type of pathology is usually treated by some specialists in Urology. It is usually done by laparoscopic surgical decompression (release of round ligaments, deitonization parallel to the ligaments, section of uterosacral ligaments, release of pudendal nerves in Alcok’s canal, ureteral isolation, of hypogastric nerves, etc.).
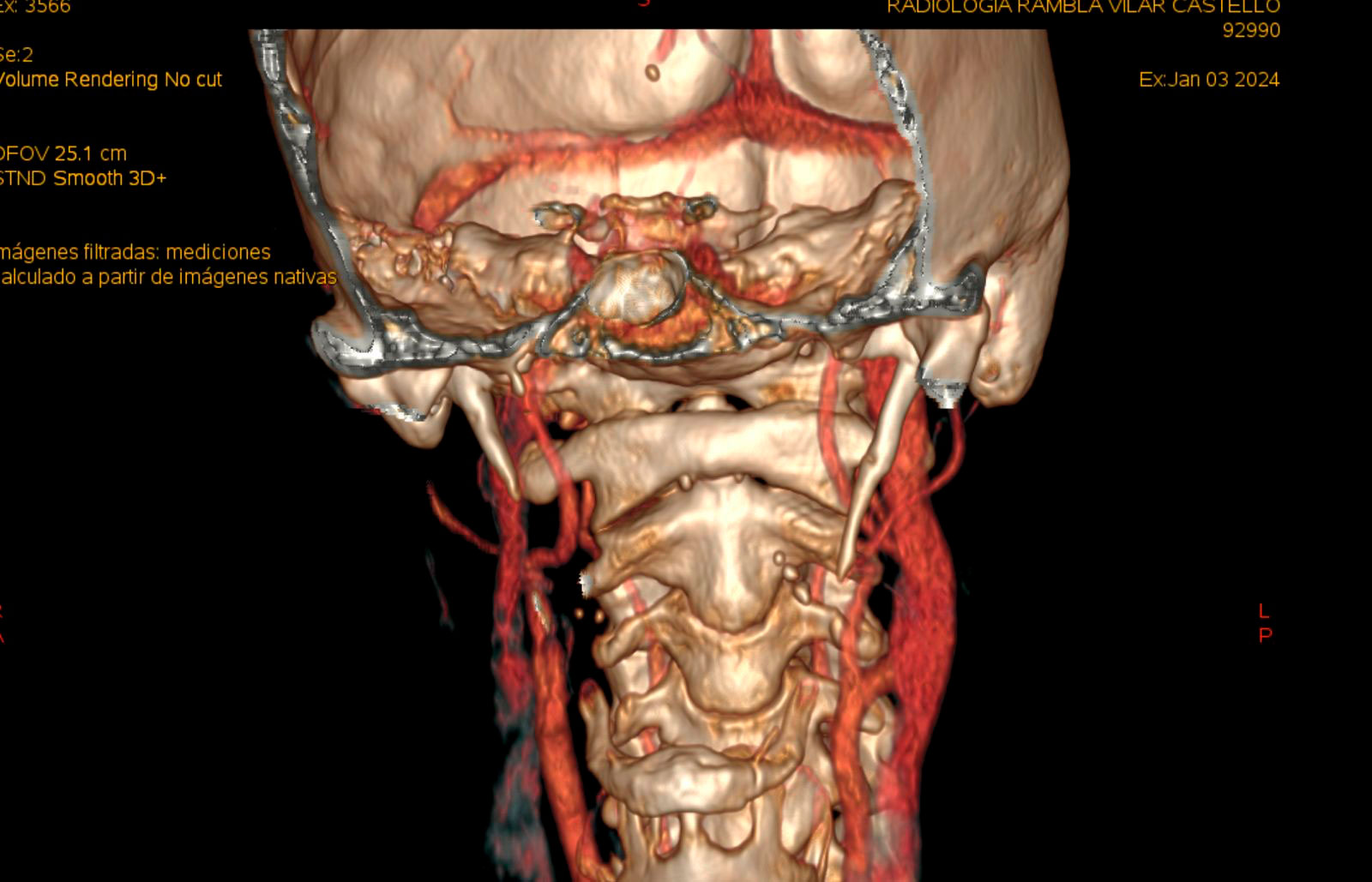
Eagle syndrome
The central focus of Eagle syndrome is the stylohyoid complex, which is composed of the styloid process, the stylohyoid ligament, and the lesser horn of the hyoid bone. In this syndrome we usually identify a styloid process that is too long (greater than 3-4 cm), although more than its length, it is its three-dimensional orientation that can compress adjacent structures (the more vertical it is, the worse).
From a symptomatic point of view, its symptoms can originate after a trauma such as a traffic accident, neck manipulation, accidental falls, tonsillectomy or tooth extraction. It usually presents as orofacial or oropharyngeal pain. During jaw movement, an “impact” occurs between the styloid and the jaw, leading to painful symptoms and difficulty moving the jaw. Its differential diagnosis is broad, including glossopharyngeal and occipital neuralgia, neuralgia, sphenopalatine neuralgia, temporomandibular disorders, dental infection, tonsillitis, mastoiditis and migraine. It can also cause vascular compression, since the styloid can compress the external carotid and its branches or the jugular vein, which leaves the skull through the jugular foramen along with some cranial nerves; which is why in our specialty (Angiology and Vascular Surgery) we frequently receive these patients.
Styloidectomy is the preferred surgical treatment option. It can be performed intraorally (advantages: no skin incision, potentially shorter operative time; disadvantages: increased risk of infection, incomplete excision of the styloid) or by laterocervical access (advantages: the process can be completely removed; disadvantages: increased risk of nerve damage, but much better vascular control).